Alzheimer’s disease (AD) begins with a long preclinical stage defined by the abnormal accumulation of amyloid-and tau proteins. These pathological proteins (biomarkers) can be measured in older adults using neuroimaging (amyloid-PET and tau PET). Transitional cognitive and neurobehavioral changes may occur during the AD pathophysiologic process prior to cognitive impairment. Identifying these transitional changes in older adults with biological markers of AD may define those at greatest risk of progression. Our research is focused on defining these transitional neurobehavioral changes in relation to brain pathology, structure and function in aging older adults. We work within the Harvard Aging Brain Study (HABS), a NIH/NIA-funded program project grant led by Drs. Reisa Sperling and Keith Johnson. HABS is an ongoing observational study of older adult volunteers with normal cognition who undergo longitudinal clinical and neuroimaging assessments. Our projects, including our HABS research, are funded by the NIH/NIA and private philanthropy.
Traditional Neuropsychiatric Symptoms and Alzheimer’s Disease Biomarkers
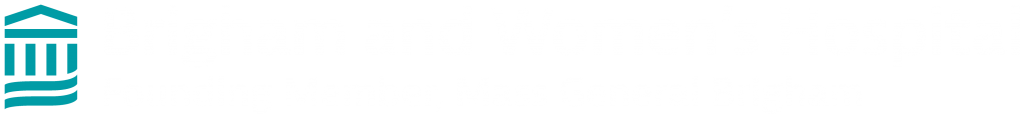
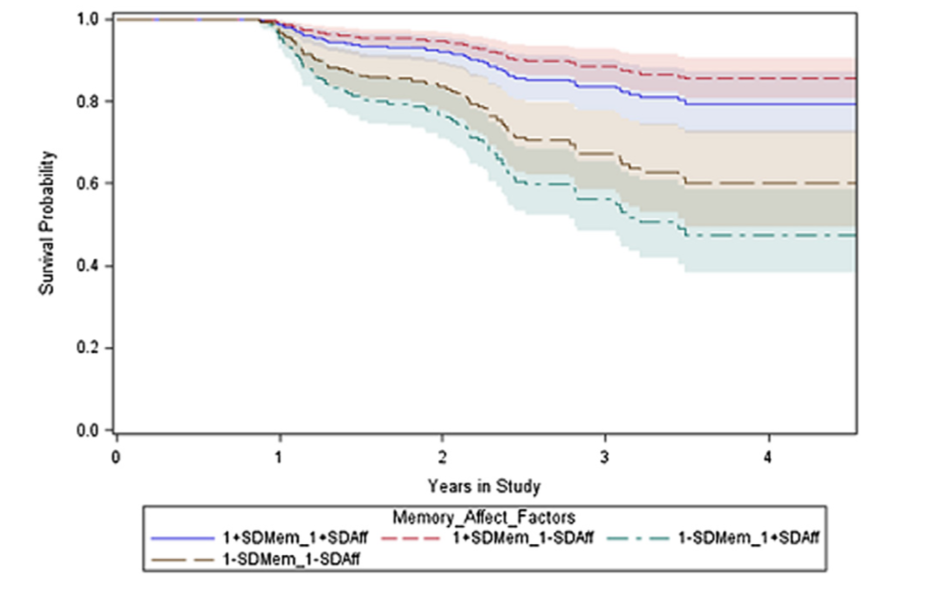
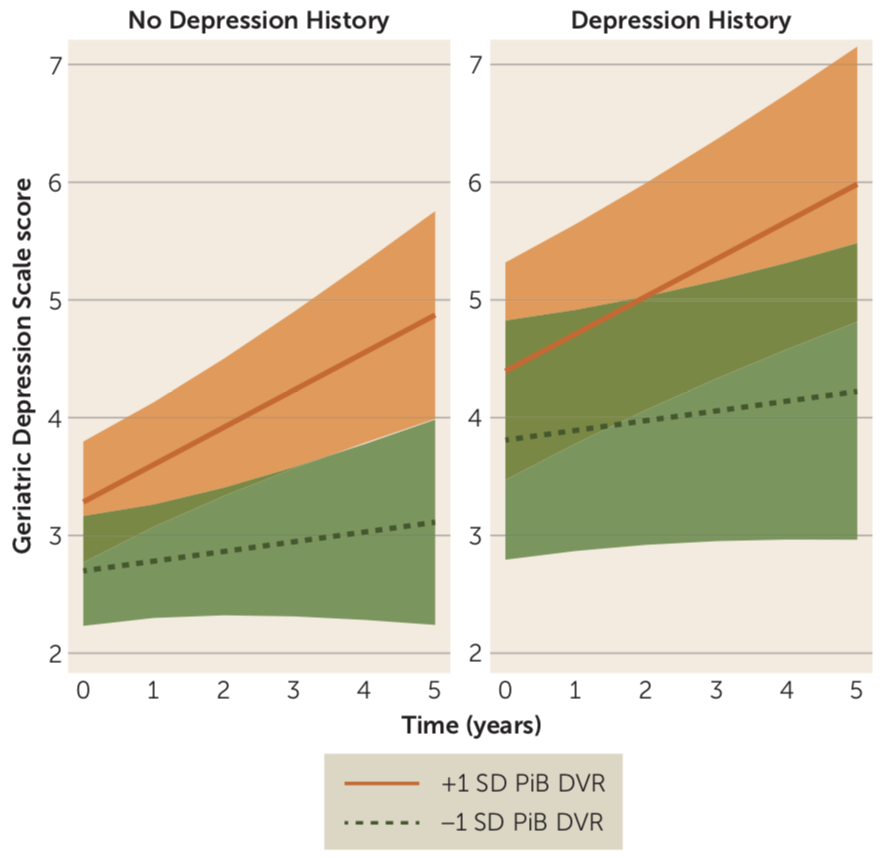
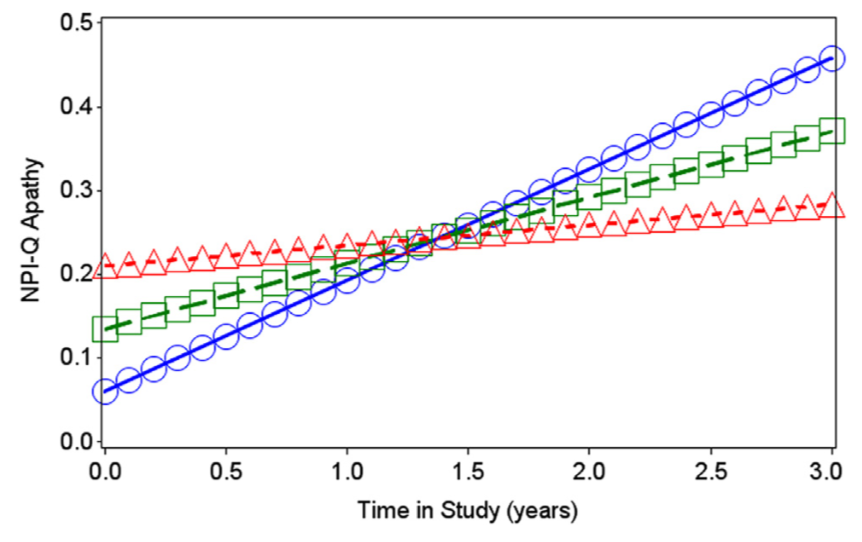
Research from our group and others has shown that a range of psychiatric symptoms such as depression, anxiety, and apathy, are associated with cognitive decline and increased risk of dementia in older adults. Our work has defined early biomarker changes associated with these traditional neuropsychiatric symptoms in normal elderly and individuals with mild cognitive impairment. Collaborators have included Dylan Kirn, Drs. Heidi Jacobs, Bernard Hanseeuw, Dorene Rentz, Rebecca Amariglio, Gad Marshall and Jennifer Gatchel.
Longitudinal Association of Amyloid Beta and Anxious-Depressive Symptoms in Cognitively Normal Older Adults (AJP 2018)
New Clues to Preclinical Alzheimer’s Disease (Rosenberg 2018 AJP commentary)
Novel Neuropsychiatric Symptoms and Alzheimer’s Disease Biomarkers
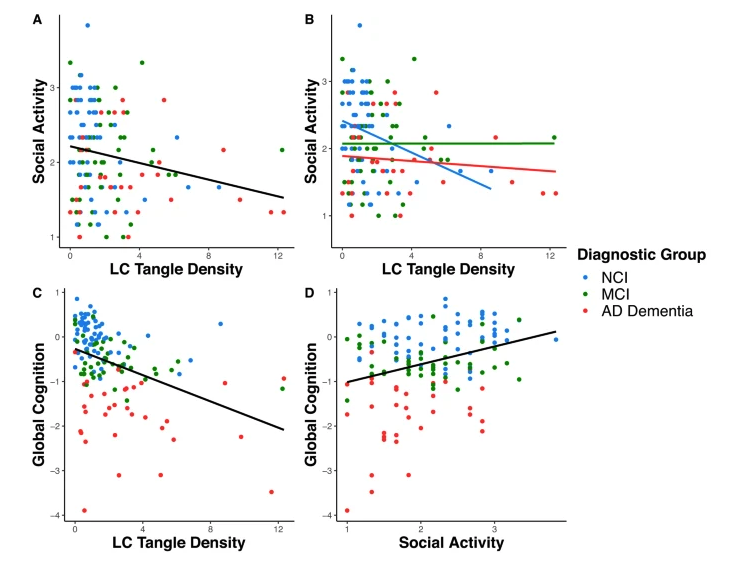
Emotional and behavioral changes in cognitively normal older people may be direct manifestations of Alzheimer disease (AD) pathophysiology at the preclinical stage, prior to the onset of mild cognitive impairment. However, relatively little is known of the natural history of these neurobehavioral changes. Our work investigates whether subjective and/or subtle objective declines in social function may be very early symptoms of AD. Recognizing these changes may enhance the identification and treatment of older individuals at high risk for progression to MCI or AD dementia.
- Loneliness and Dementia in Context (American Journal of Geriatric Psychiatry, 2023)
- Loneliness: Science and Practice (American Psychiatric Association Publishing, 2023)
- Social disconnection in older adults with Alzheimer’s disease and other neurodegenerative conditions, NIMH Social Disconnection in Late-Life Suicide Workshop (Presented at NIMH Conference, 2020. Click to view talk on Youtube)
- Social Isolation and Loneliness in Older Adults: Review and Commentary of a National Academies Report (American Journal of Geriatric Psychiatry, 2020)
- Timely Insights into the Treatment of Social Disconnection in Lonely, Homebound Older Adults (American Journal of Geriatric Psychiatry, 2020)
- Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System (National Academy of Science, Engineering and Medicine, 2020)
- Regional Tau Pathology and Loneliness in Cognitively Normal Older Adults (Translational Psychiatry 2018)
- Association of Higher Cortical Amyloid Burden With Loneliness in Cognitively Normal Older Adults (JAMA Psychiatry 2016)
- Loneliness as a Marker of Brain Amyloid Burden and Preclinical Alzheimer Disease (Rosenberg JAMA Psychiatry 2016 Commentary)
- Loneliness, depression and cognitive function in older U.S. adults (IJGP 2016)
Interventions for Socioemotional Wellbeing
During the Covid-19 pandemic, we initiated new pilot studies to investigate interventions to address loneliness in community dwelling older adults. You can find information on our Music Therapy study and Intergenerational Friendly Telephone Visits below.
A Study of Virtual (Zoom) Music Therapy for Older Adults Living Alone:
Music therapy has been shown to improve physical and mental health and quality of life for older adults. This may be an important tool during the coronavirus pandemic when many people felt disconnected from others. This pilot study enrolled 8 older adults who were living alone and evaluated the impact of music therapy on feelings of social connection, stress and other aspects of mental health.
A Study of Friendly Telephone Visits with Older Adults:
Friendly phone visits between older adults and younger generations have become very popular, but little is known about what may make these worthwhile or helpful for those involved. This was especially relevant during the coronavirus pandemic when many people experience feelings of disconnection from others. To investigate this, we evaluated the experience of 10 older adults who were matched up with 10 undergraduate students for friendly phone visits. We were specifically interested in those who were living alone and experiencing feelings of loneliness during the coronavirus pandemic.
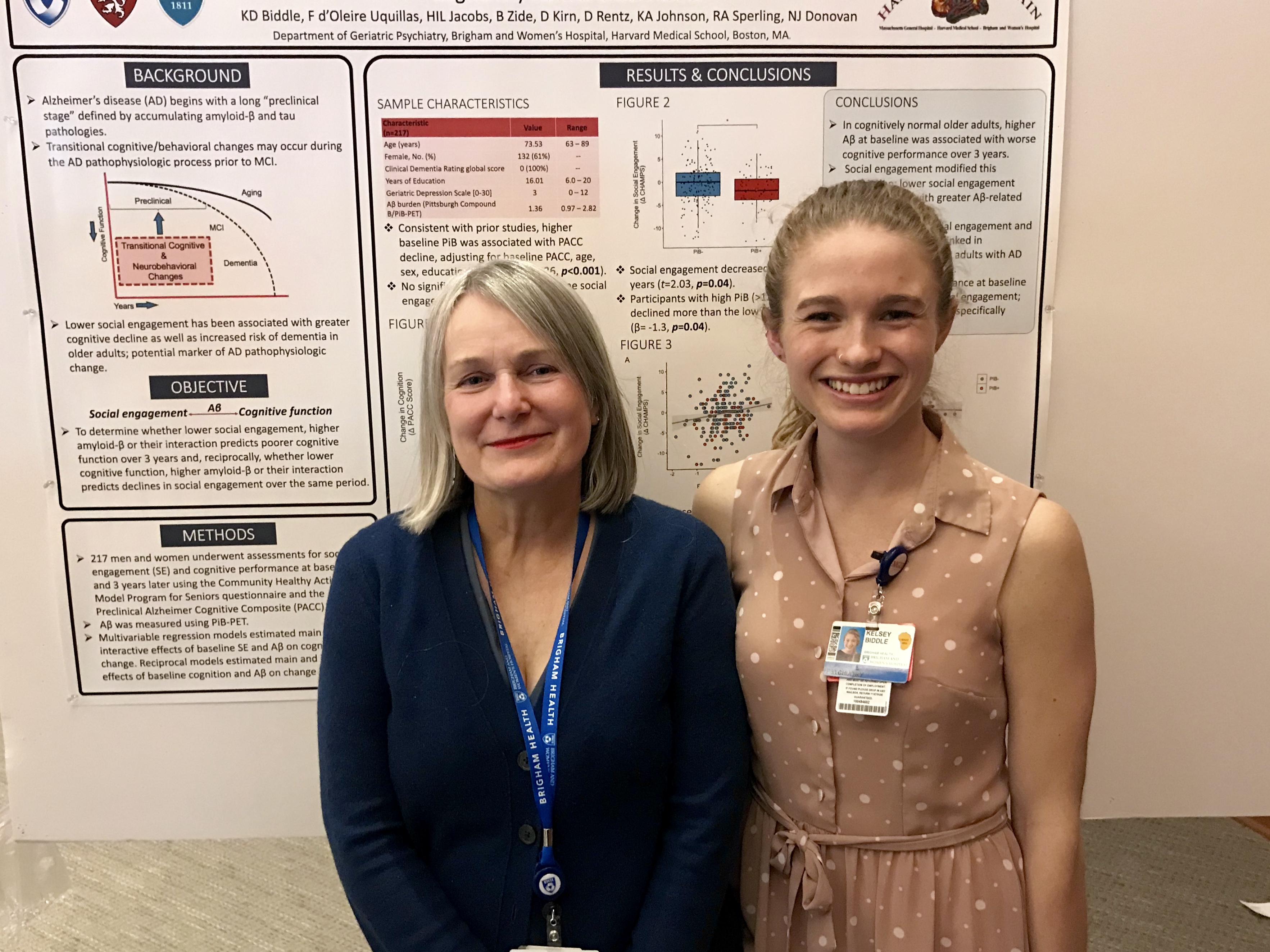
As part of her elective MS3 research year, HMS student Kelsey Biddle led a new pilot study to investigate the feasibility and value of a storytelling-based intervention for adults with early cognitive impairment. You can find information on our Narrative Medicine study below.
A Personalize Narrative-Based Intervention for Adults with Early Cognitive Impairment and their Care Partners:
Storytelling is fundamental human activity that can serve as a tool for personal growth and making sense of life challenges. We are interested to learn if writing and talking about experience(s) with early cognitive impairment, facilitated by a train health coach, can help people process and cope with the challenges of early-stage cognitive impairment. This pilot study will enroll 12 dyads of adults with early cognitive impairment and their care partners to evaluate the experience and perceived benefit of narrative-based practices in older adults with cognitive impairment.
EXPLORE
If you’re interested in learning more about this area of Alzheimer’s Disease research, here are links to relevant scientific articles from thought leaders in the field.
PET staging of amyloidosis using striatum (Hanseeuw BJ et al., Alzheimer’s and Dementia, 2018)
For more information about Alzheimer’s Disease and aging, go to: https://www.nia.nih.gov/
FUNDING & ACKNOWLEDGEMENTS
Our research has received funding from the following sources:
- HMS Dupont Warren and Livingston Fellowships (2013-16)
- NIA R03AGO45080 (2013-2016)
- Alzheimer’s Disease Neuropsychiatric Research Fund (2015- present)
- NIA R21AG054953 (2017- 2021)
- Healthy Aging Research Fund (2017-2022)
- Older Adult Covid Relief Fund (2020-2022)
- Neuropsychiatry of Aging Fund (2022 – 2025)
- Geriatric Psychiatry Fund (2022 – 2025)
Our research is possible through the collaboration and support from our colleagues at the Harvard Aging Brain Study. Thank you to the entire Harvard Aging Brain team and to our study participants.
Reisa Sperling, MD, Keith Johnson, MD, Dorene Rentz, PsyD, Rebecca Amariglio, PhD, J. Alex Becker, PhD, Rebecca Betensky, PhD, Deborah Blacker, MD, Rachel Buckley, PhD, Randy Buckner, PhD, Jasmeer Chhatwal, MD, PhD, Brad Dickerson, MD, Michelle Farrell, PhD, Jennifer Gatchel, MD, PhD, Stephen Gomperts, MD, PhD, Doug Greve, PhD, Edmarie Guzman-Velez, PhD, Bernard Hanseeuw, MD, PhD, PhD, Brad Hyman, MD, PhD, Heidi Jacobs, PhD, Cristina Lois, PhD, Gad Marshall, MD, Scott McGinnis, MD, Beth Mormino, PhD, Kate Papp, PhD, Enmanuel Pardilla-Delgado, PhD, Cleofe Peña Gomez, PhD, Julie Price, PhD, Deepti Putcha, PhD, Yakeel Quiroz, PhD, Jennifer Rabin, PhD, Liliana Ramirez Gomez, MD, Aaron Schultz, PhD, Dennis Selkoe, MD, Jorge Sepulcre, MD, Sietske Sikkes, PhD, Patrizia Vannini, PhD, Hyun-Sik Yang, MD, Wai-Ying Yau, MD; Arabiye Artola, Clara Castelar, Tobias Estime, Colleen Fitzpatrick, Josh Fuller, Olivia Hampton, David Jin, Samantha Katz, Emily Kilpatrick, Justin Kim, Dylan Kirn, Hannah Klein, Evelyn Luner, Lyssa Manning, Hana Markova, Danielle Mayblyum, Kirsten Moody, Martha Muniz, Irina Orlovsky, Michael Properzi, Alejandra Restrepo, Aubryn Samaroo, Justin Sanchez, Matthew Scott, Amanda Sidwell, Paige Sparks, Heirangi Torrico-Teave, Steven Weise.